It’s open enrollment. Are you prepared?
 Year after year, most employees just renew the same health benefit plans they had the year before. Up until this open enrollment season, that was good news for you. But the pandemic has heightened employees’ health concerns and the importance they place on employer-provided health benefits. Employees who chose skimpier plans last year may feel those benefits are inadequate now.
Year after year, most employees just renew the same health benefit plans they had the year before. Up until this open enrollment season, that was good news for you. But the pandemic has heightened employees’ health concerns and the importance they place on employer-provided health benefits. Employees who chose skimpier plans last year may feel those benefits are inadequate now.
A little employee outreach now can make employees savvier about their health plan options.
Help employees overcome health benefit illiteracy
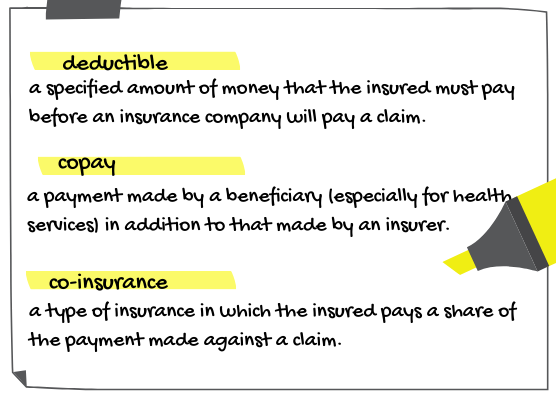
You can eliminate some of the questions employee will have by making sure they know the lingo. What’s the difference between a co-pay and coinsurance? What’s balance billing?
Health plans must provide employees with a summary of benefits and coverage and a glossary of health benefit terms. Odds are, employees just toss those documents in a drawer.
Tip: Pull out the most common terms from the glossary—deductible, co-pay and co-insurance—and highlight them separately in your communications materials.
Going virtual
Employees probably aren’t going to be able to walk into your office with questions. And you may not be able to make your benefits pitch in person this year, either.
Working with your group health insurer can get you over some hurdles. Your insurer may be able to set up a virtual benefits fair for employees. A virtual benefit fair platform usually has a virtual lobby, exhibit hall and video vault. Employees can go online to make their benefits selections.
Alternatively, you can schedule Zoom or Google Meets meetings with whole departments first. Then use a scheduling tool for meetings with individual employees, later. If you’re uncomfortable with video, webinar platforms or Slack offer alternatives. If you use a slide deck, keep the slides simple (we’ve read no more than 12 words per slide) and concentrate on new offerings.
Open the toolbox
You’re probably still going to mail information packets to employees. But also consider other communications tools, which are readily adaptable to virtual environments:
- Use email, posting to social media websites and easy-to-use web-based calculators and tools. Don’t bury important information three screens down from the homepage.
- Use FAQs to communicate changes to current health benefits, such as the increase in employees’ pretax deductions and the new inflation-adjusted contribution amount into health FSAs. Tips: Employees may be reluctant to use their home printers to print your FAQs, so keep them as short and possible and eliminate colorful graphs, screen shots, stickers, etc. Also be sure to include a reply email address for employees who have follow-up questions.
Keep it simple, personal and familial
New options need a more coordinated roll out. The material you provide to employees should be written as simply as possible.
Tip: Since health insurers’ brochures often fall short of the keep-it-simple rule, create supplementary materials showing how typical employees like them would fare among the various options. Don’t undersell cost-shifting mechanisms like co-pays; doing so can leave employees feeling like they were shortchanged.
Spouses and significant others may be the ones who handle the health care decisions or schedule doctors’ appointments. Tip: Mail home the same information employees received at meetings.
Be patient
Don’t dump materials on employees and expect them to read everything right away. Tell them to take the time to review all that information. They’ll have questions about new plans and new plan options. Expect an increase in emails after employees and their spouses have a weekend to dig through the material you’ve provided.
As for the open enrollment process itself, don’t pick Friday as the enrollment deadline. Why: Friday deadlines only increase Monday morning phone emails. Wednesdays seem to be best.
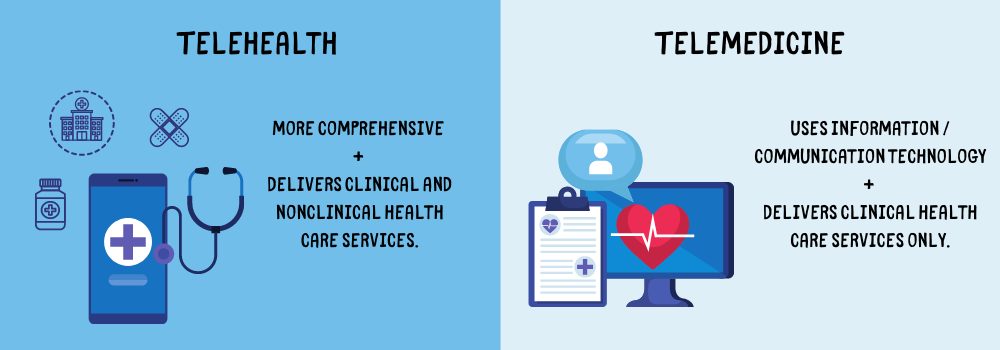
Telehealth vs. telemedicine
Although telehealth and telemedicine sound the same, they aren’t, at least under federal law. If your introducting these in your open enrollment package, or just want to highlight them in your communications this year, here’s a quick breakdown:
- Telehealth is more comprehensive and generally refers to a health care provider’s use of information and communication technology to deliver clinical and nonclinical health care services.
- Telemedicine generally refers to a health care provider’s use of information and communication technology to deliver clinical health care services only.
Acceptance of telehealth may be generational—younger employees who are smartphone-savvy may be more amenable to it than older employees. Which means you may have to sell it to a chunk of your workforce.